When I turned 43 a couple of months ago, I noticed something was… different. Not just the tinsel of gray hairs poking out from my scalp or the disordered sleep I was suddenly experiencing, but something more frustrating for a woman who writes about sex for a living: my libido. I felt disconnected. I wasn’t as horny as I used to be and, needless to say, I was annoyed.
“Great, now I have to worry about sex too?” I thought, mentally adding it to the growing list of perimenopause grievances.
But here’s the thing: A change in sex drive, as daunting as it can feel initially, is completely normal as we age — and it doesn’t have to be a negative thing.
“So many women in perimenopause feel like something is ‘wrong’ with them because they’ve been sold a completely unrealistic story about female desire,” Dr. Vanessa Coppola, a menopause expert and founder of Bare Aesthetic and Bare Soul Wellness, tells Scary Mommy. “You’re supposed to want sex the same way you did at 25 for the rest of your life, and if you don’t, it must mean you’re broken or your relationship is failing.”
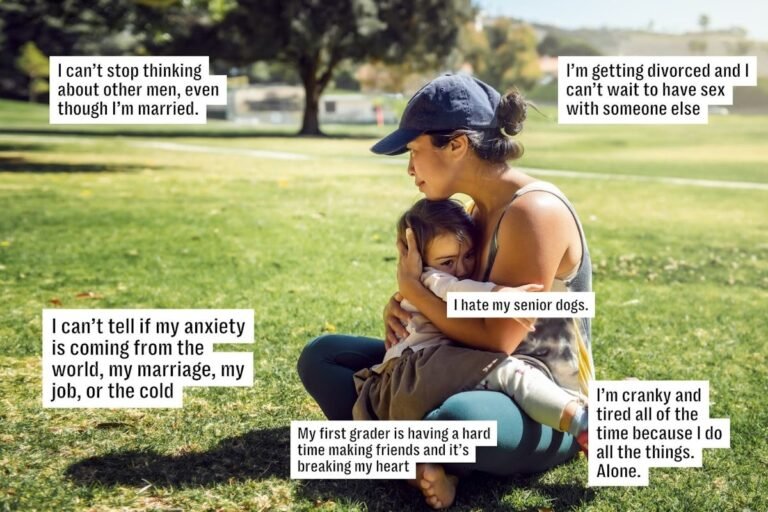
What’s actually happening, Coppola explains, is much more biological. During perimenopause, sleep can become fragmented, which shifts brain chemistry: dopamine drops, cortisol rises, and the nervous system becomes less available for pleasure. Estrogen fluctuations affect mood, tissue comfort, and arousal response. Add in the rising mental load many women carry in midlife — work, caregiving, household responsibility, constant decision fatigue — and libido often becomes quieter, slower, and less spontaneous.
“It’s not a flaw,” she adds. “It’s your body adapting, and it can even open the door to a more mindful, intentional, and ultimately satisfying sex life — just in a different way than it used to be.”
Understanding what’s happening to your sex drive can empower women to navigate desire without shame or self-doubt. Here’s what the experts have to say.
The 30s
In your 30s, many women experience what Alicia Sinclair, sex educator and founder of Le Wand, calls a “sexual confidence peak.” “You know your body better, you’re more comfortable communicating your needs, and you’ve often shed some of the shame or insecurity from your 20s,” she explains.
But confidence doesn’t always translate to desire. Life pressures — from career to caregiving to parenthood — can complicate libido. Sinclair notes, “Even if desire is still robust, sleep deprivation, stress, and parenting responsibilities can really dampen it.”
Coppola echoes this, emphasizing that desire becomes less spontaneous with age. “You might not wake up wanting sex as easily as you did in your 20s,” she says. “It’s not that something is broken; your libido is just more context-dependent now.”
The 40s
Here’s where your sex drive can feel especially unpredictable. Perimenopause often begins in the 40s, bringing major hormonal volatility. Sinclair explains, “Some women experience a temporary increase in desire early in perimenopause, while others notice a decline.” (More on that below.)
Lisa Finn, sex educator with Babeland, highlights the physical effects of estrogen loss. “Dropping estrogen can lead to vaginal dryness, less elasticity in the pelvic floor, and sometimes pain during intercourse,” she says. “These changes make sex less comfortable, but pleasure is still possible with adaptation and communication.”
Coppola explains why desire often feels so erratic: “Estradiol can spike and crash unpredictably, progesterone often drops earlier, and the nervous system becomes more reactive, leading to sleep disruption, anxiety, and mood symptoms that directly impact sexual desire.”
Stress and mental load also matter. “Women in their 40s are juggling careers, families, and aging parents,” Sinclair notes. “Even if hormones are fine, chronic stress and sleep disruption can override sexual interest.” Coppola calls this “survival mode”: the body prioritizes energy for life demands rather than pleasure, which isn’t a reflection of sexuality; it’s physiology.
“So many women tell me, ‘I want to want sex, but my body doesn’t respond,’” says Coppola. “That’s often tissue plus nervous system biology. And here’s the relief: When we treat dryness, pain, and sleep disruption, desire often returns far more than women expect.”
The 50s
By the 50s, many women are post-menopausal, with lower baseline estrogen and testosterone. “Some women feel relief — less fear of pregnancy, increased confidence — while others experience decreased desire due to estrogen depletion, vaginal dryness/pain, and lowered androgen activity,” Coppola explains.
In other words, libido can vary widely.
Estrogen supports libido indirectly by maintaining vaginal tissue integrity, blood flow, lubrication, and comfort. “When estrogen declines, women often develop genitourinary syndrome of menopause (GSM), experiencing dryness, burning, recurrent UTIs, and dyspareunia, which can condition the brain to associate sex with discomfort,” Coppola says. “That alone can suppress desire.”
Testosterone plays a more direct role in sexual motivation and arousal. “Women produce testosterone via the ovaries and adrenal glands, and levels gradually decline with age. During the menopause transition, the issue isn’t always absolute testosterone deficiency; often, estrogen loss causes pain and reduced arousal response, which women interpret as a ‘loss of libido,’” Coppola explains.
“For many women, desire doesn’t disappear; it just stops showing up ‘randomly’ and starts requiring the right conditions,” she adds. “That shift is incredibly common, and it’s also workable.”
Sinclair agrees: “Spontaneous desire often decreases, but that doesn’t mean desire disappears. Many women report their sex lives actually improve because they have more time, less worry about pregnancy, and a clearer sense of what brings them pleasure.”
Why so many perimenopausal women believe their sex life is broken
When your body stops responding the way it used to, it’s easy to assume something is wrong.
Finn encourages reframing the experience: “Think of these changes not as limitations, but as invitations to start fresh and rediscover new ways to explore and enjoy sensation. In fact, taking the time to be mindful about your sexual desire and pleasure through perimenopause and menopausal changes can allow us to truly become better in touch with ourselves, discovering and unlocking new routes for pleasure and orgasm.”
Dr. Beverly Joyce, sexual wellness coach and HotPause Health advisor, adds that much of the distress comes from unrealistic expectations. “Because nobody told them what ‘normal’ can look like in midlife, many women have been sold the idea that desire should be spontaneous, automatic, and easy. When it becomes more conditional on sleep, stress, time, and comfort, they assume something is broken,” she says.
“What I see clinically is that a lot of women are experiencing completely predictable changes like sleep disruption, mood changes, body changes, and vaginal symptoms, but they’re interpreting it as a personal failure,” Joyce continues. “If sex becomes uncomfortable because of [menopausal symptoms], the body often shifts into avoidance mode. That’s not broken, that’s biology doing its job. The ‘fix’ often starts with addressing pain, dryness, and the pressure to perform.”
What you can do about your libido
Your sex life is not lost during this stage of life. You can love sex again. You can feel desirable again. There are real solutions, says Coppola, and you don’t have to just “accept” having a low libido.
Some practical ways to support midlife desire:
- Address vaginal health: “If sex is painful or uncomfortable, desire will naturally decrease,” says Sinclair. “Vaginal moisturizers and lubricants are essential. For more significant vaginal atrophy, low-dose vaginal estrogen is highly effective and has minimal systemic absorption.”
- Stay sexually active: Sinclair notes, “The ‘use it or lose it’ principle actually has merit — regular arousal and orgasm support blood flow and tissue health. Vibrators and personal massagers can be especially helpful.”
- Prioritize responsive desire: “Instead of waiting to ‘feel like it,’ try engaging in pleasurable touch and seeing if desire emerges. This responsive desire pattern is completely normal and valid,” Sinclair says.
- Strengthen your pelvic floor: “A pelvic floor PT can address pain, tension, or weakness that affects sexual function. This is underutilized but incredibly effective,” Sinclair adds.
- Support the nervous system: Joyce says, “No single food or supplement reliably ‘restores libido.’ What helps most consistently are the fundamentals that support the nervous system and body image: sleep, movement (especially strength training), and stress reduction.” Sleep is especially crucial. “Many women underestimate how much insomnia and night waking blunt desire. Movement helps mood, energy, and body confidence. Chronic stress keeps the body in a defensive state where desire is harder to access.”
The question you really need to ask yourself
And remember: “normal” is relative.
Joyce emphasizes that “there is no single ‘correct’ trajectory for libido. Some women feel steady desire across decades, some feel an uptick, and some feel a decline — and all of that can be normal. What we do see in research is that low sexual desire becomes more common during the perimenopause transition and after menopause, especially when symptoms like poor sleep, hot flashes, mood shifts, and vaginal discomfort enter the picture.”
She adds a reassuring data point: “In a large U.S. study, about 27% of premenopausal women reported low sexual desire, compared with about 52% of naturally menopausal women. The most important clinical question isn’t ‘Is my desire lower than it used to be?’ It’s ‘Is this change distressing to me, affecting my relationship, or making me feel unlike myself?’ Because that is when we can help.”