In the “Golden Age” of antibiotic discovery during the 1950s and ’60s, pharmaceutical companies, research institutions and scientists joined forces in a global hunt for life-saving compounds. They scoured soil samples from the Amazon to the Himalayas, exchanged microbial strains across institutions, and shared discoveries — like Streptomycin, the first effective treatment for tuberculosis — within weeks, a previously unprecedented pace. It was a time when science advanced rapidly through remarkable openness and collaboration.
In the decades since, antibiotic resistance has grown into a full-blown crisis — not for lack of scientific know-how or effort, but because of deeper structural challenges. Still, the collaborative spirit of that era offers a powerful model for how we can respond.
According to the World Health Organization, antimicrobial resistance is one of the top 10 global public health threats facing humanity, yet only a handful of new antibiotics have been approved in recent years. With limited financial upside, small, mission-driven teams are now carrying the torch for antibiotic discovery — working with a fraction of the resources and an ever-growing demand for high-quality data. Today, just three major pharmaceutical companies continue to maintain antibiotic discovery programs, as the vast majority have exited the field.
Most new antibiotics earn less than $50 million per year, despite treating millions. Meanwhile, other areas of medicine can generate billions annually, often while serving smaller patient populations. This disparity highlights how market incentives don’t always align with urgent public health needs.
Already, antibiotic resistance is responsible for over 1.27 million deaths annually — contributing to nearly 5 million deaths in total — and without intervention, it risks becoming one of the leading causes of death worldwide by 2050.
AI holds real promise to reverse this trend. By quickly generating novel compounds in a rapid feedback loop with experimental validation, AI can cut down on both time and cost — reducing failed experiments and enabling fewer, but better, “shots on goal.” But even the most advanced algorithms can’t deliver results without something foundational: data.
Despite AI’s potential, most small biotechs face a formidable obstacle: a scarcity of accessible, high-quality data. Training effective AI models requires tens of thousands of data points, each costing around $50 to generate. That’s $5 million just to get started. For startups working in low-margin fields like antibiotics, that’s often out of reach.
At Phare Bio, we’ve experienced these bottlenecks firsthand.
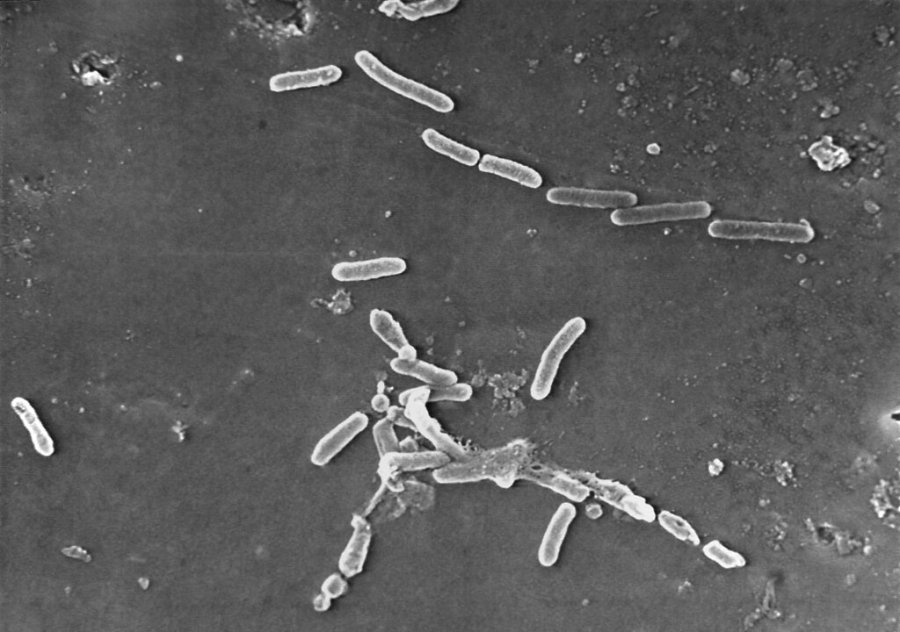
In our early days, we relied on predictive AI models to identify antibiotic properties across existing libraries of millions to billions of compounds. It was during this period that our academic partners at MIT’s Collins Lab discovered the first novel antibiotic class using AI.
But even then, our ability to generate promising leads was outpacing the data available to support meaningful discovery. Many of the datasets we relied on had already been heavily mined by other researchers, limiting the novelty of findings and potential for new intellectual property.
Today, we’re charting our own course using generative AI to propose entirely new chemical structures — novel, drug-like compounds to combat the world’s deadliest superbugs. This approach has already led to two additional novel antibiotic classes, accelerating our pace, precision and scale. Yet we still lack the data to keep up with our model’s potential.
So, with government and philanthropic support, we’ve been generating our own datasets, aggregating public data, and building lean workflows to stretch every dollar. We’ve created a viable economic path — and we’re committed to open-sourcing much of the data we generate to help others do the same. But we could move even faster if we could galvanize broad data-sharing efforts across the field.
Data sharing doesn’t have to mean giving up control. In fact, AI and cloud technologies have made it easier than ever to collaborate responsibly. Federated learning allows for model training without data leaving its source. Time-limited agreements and anonymized training protocols help ensure security without exposing proprietary data.
We’ve already seen how secure, coordinated data-sharing can accelerate scientific progress. The Protein Data Bank, for example, has enabled decades of breakthroughs by making structural data on proteins freely available to researchers worldwide.
Imagine a world where biotechs can securely train better models using each other’s data — without it leaving individual platforms and with full transparency around how it’s used. Where big pharmaceutical companies lend or license dormant, non-sensitive data to small biotechs, especially in areas with limited financial upside or persistent scientific gaps, fueling the discovery of new drug leads in therapeutic areas of unmet need.
Unlike traditional partnerships that often occur later in the drug development process and behind closed doors, this model draws from open science principles — encouraging early-stage data-sharing, decentralized collaboration, and shared infrastructure to accelerate discovery. In return, pharma companies can license the most promising compounds and take them through preclinical and clinical development — or support biotechs in advancing them. Startups get data and capital to advance programs. Pharma re-engages in once-abandoned fields with de-risked assets. And most importantly, patients get faster access to urgently needed, life-saving drugs.
We’re fighting 21st-century battles with 20th-century tools. As we increasingly pair machine and human intelligence to powerful effect, we are in a transformative moment where open science could once again unlock a sea change in biotechnology.
We must revive the Golden Age of drug discovery: collaborative, pragmatic, urgent. The stakes are too high to remain siloed.
The data is out there. Let’s use it to save lives.
Akhila Kosaraju, M.D., is president and CEO of Phare Bio — a biotech social venture leveraging generative AI to discover the next generation of novel antibiotics.